The concept of ‘was that my last good day’ is a permanent spectre in my life. I no longer get as rattled by the unpredictability in quite the way that I used to, but it never really goes away. For example: I had an amazing weekend just gone. I Walked 29km over two days, went to a pub for the first time since lockdown, baked some fresh bread, saw friends etc. And now, Monday morning, I wake feeling a bit weird and a bit off. Hard to explain but my mood is one of inexplicable hopelessness, I feel shattered already and am generally quite sub-par. Go figure.
One of the stranger things about having MS is that you just have to accept is the complete unpredictability of it all. Hot/cold, happy/sad, pain/no pain. see/double vision, you get the idea. If you don’t I reckon you’ll go stark staring mad in a matter of months. But back to the present wobble…
All of a sudden, across my mind, flits the well worn thought of, ‘was that it’. Rational Me knows that this is ridiculous. Still, rationality takes a back seat and Irrational Me triumphs. I know this is a bad and dark hole to allow myself to be dragged into and it is a Herculean effort to force Rational Me back and send it on the daily task of kicking all the silly Irrational Me thoughts and fears back into the dark recess where I think they ought to stay.
Talking of dark holes, these are the parts of the mind that don’t show up on my MRI and are not easily quantifiable to my neurologist. They are impossibly hard to describe and when I get to my once annual review they seem like an odd abstract thought that, in trying vainly to describe, will take away from that valued visit for the ‘serious stuff’, making me loath to spend those precious minutes trying to explain the inexplicable.
There are so many things to measure with MS, and the neurologists want to hear about them because that is an efficient clinic visit. Recording the measurables. How well you walk, pee, see, swallow, and so on. They like those sort of metrics as they can place you somewhere, measure stability or decline and tell you where you are in the journey of decline. The anxiety stuff? The demons, the black feelings and so on? Most prefer to leave that to the staff of P-Wing because there is no EDSS equivalent that can describe the daily rollercoaster of emotions, that’s life. I always leave feeling as if everything that has been said is caveated with the equivalent of a warning on an investment product about the past performance being no guarantee of the future.
Annoying as that is to both parties, in Multiple Sclerosis there has never really been a way to look into the future and reliably predict either the potential onset, extent, and/or severity of the illness in general or the relapses that characterise the earlier stages of the disease. So when they say that it is impossible to tell, they aren’t joking. Watch and wait is their motto. Hope and pray is mine. Either way, both are as uncertain as the other. They can measure what has happened or, at best, what is happening, and in fairness, who likes dealing in the what-ifs and the maybes? I imagine that every neurologist that has ever had to deliver a diagnosis of MS to some poor soul has been met with a version of, “what is going to happen to me?” and it is a very difficult question to answer. The ability to quantify anything with regards to that question is v tricky, and, in general, by the time a doctor has made it to the heady heights of Consultant they are well-versed in the delivery of difficult messages such as, hmmm, not sure really, we’ll have to wait and see. No looking into the future here. Move along.
But there are some glimmers of hope! Whilst there isn’t the precision that I or my neurologist may want, these days there are tools that offer the opportunity to go beyond an educated guess.
I can think of three emerging tools that give real hope for taking a forward view. Neurofilament Lightchains (NfL’s), Optical Coherence Tomography (OCT), and Artificial Intelligence (AI) analysis of MRI.
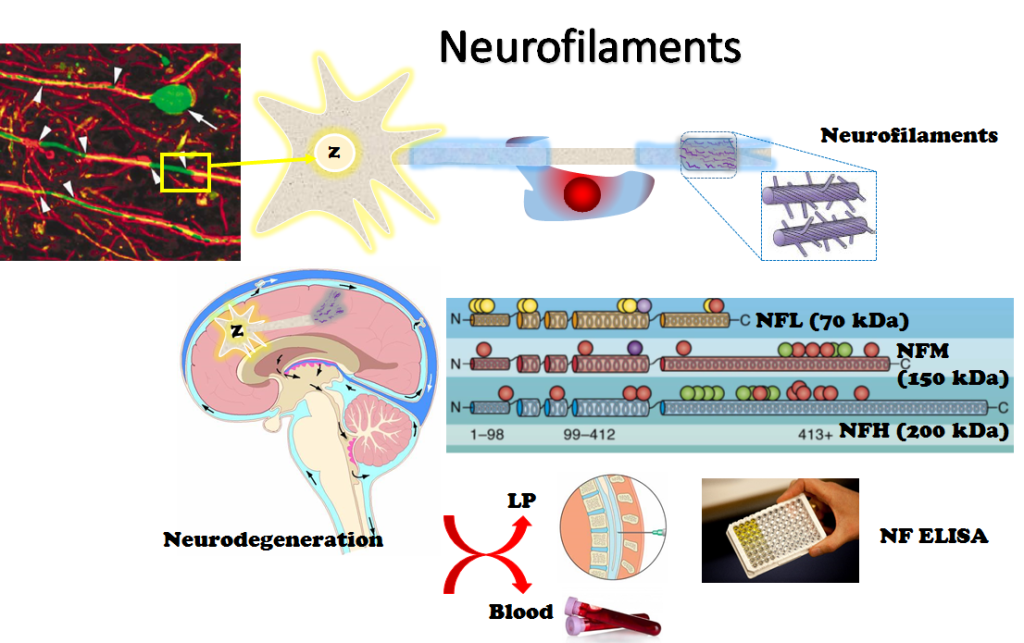
1 – Starting with NfL’s, these are things that can be taken from the fluid that is drained during a lumbar puncture. They serve as biomarkers, a fancy way of saying signposts from our body, regarding three main things:
- Risk of progression. E.g.: The how bad is this going to be doc, question?
- Clinical disease activity. Not what you can or can’t see/elicit from patient recollection of symptoms or tests done to determine the level of effect at the time but what is actually going on in my noggin.
- Treatment response. Have you ever wondered if the DMT you are on is doing anything? I have a standard reply to people when they ask about DMTs for MS. I explain that unlike a paracetamol that does or doesn’t fix a pain, the DMT is taken with a belief in science and large scale clinical trials. They say it works and I have to believe that.The neurologists are in the same boat. We all have to believe in science that a good DMT increases the time between relapses and reduces the effects of a relapse when we do have them. We will, it is a progressive illness. A very rare few may experience no measurable progression in life. They are the exception that proves the rule.
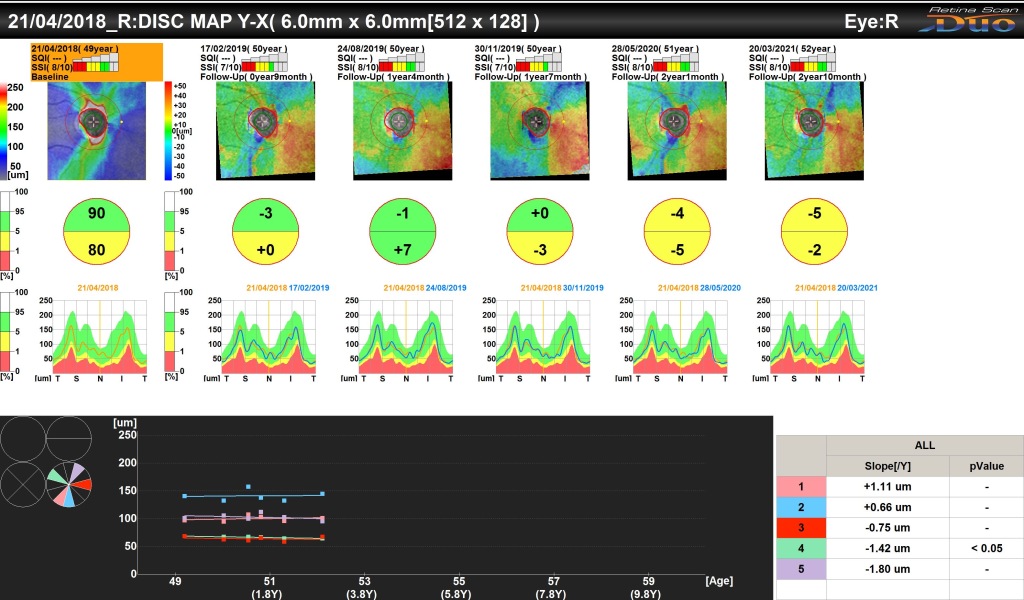
2 – OCT scans are a bit like looking into a supermarket barcode scanner when you have one. It feels like little bars of red light flitting around trying to determine the price of your eyes! What comes out though is amazing. They map the retina thickness and condition and compiled over time they allow an expert to see into the brain through the eyes. The presence or loss of ganglion cells (I am emphatically not an expert) also serve to let the doctor know what is happening in the brains of the patient. When they are done as a matter of course (not right now) they’ll also need someone to understand and interpret them, or they are pointless – this probably isn’t going to be your neurologist.
Presently, it still does not make a difference for the clinical management. But it’s very promising and much more convenient than brain volume measurements on MRI, and is probably going become very important in the future.
This is a very promising biomarker as it is easily accessible and reflects brain damage and will allow the neurologist to quantify how neuroprotective a treatment is.

3 – Finally, AI examination of MRI scans is allowing doctors to identify different manifestations of MS. By seeing these they can better understand what is more likely to happen. An added bonus is that once a computer is sufficiently well trained and is running the right software it can be relentless. Humans get tired, need coffee, are distracted, miss things, misinterpret things, however diligent we are. People try their best but it is a boring and repetitive task gazing at slice after slice after slice of an MRI. To have a computer do that heavy lifting is infinitely preferable. This means that the human expert neuroradiologists get notified of the results and can verify and check the anomalies a computer picks-up that may go unnoticed to a human being, however good they are.

If you aren’t a little in awe by now then you need to get checked. This is amazing. For the very first time, there are tools and technologies that will allow our doctors to treat us for what they know is going to happen and not what they think might happen. It is the moving to precision treatment and not hitting everything with the biggest hammer they can lay their hands on. It is allowing patients to understand why their neurologists offer the choices they do and say some of the things they do. These days, only the most backward neurologists think MS is an on/off sort of disease. To say you aren’t progressing is inaccurate. A better phrase is, ‘with the tech we have available we can’t see anything at the moment.’
These tools are years away, not decades. The next time I see my neurologist I’ll be asking them how they think they’ll be deploying these technologies to treat me better? As for the mental strains, I still don’t know where to begin with these. I have found that it is likely to remain my job for a long time to come. But things do get a little easier when we know a bit more about what is around the corner. Go science!
With thanks to Dr Sharmilee Gnanapavan (@neurognanapavan) and Dr Ide Smets (@SmetsIde) for ensuring I wasn’t talking total rubbish.
For some more in-depth reading there are links to some of the most recent work:
NfL’s – https://multiple-sclerosis-research.org/2021/04/do-you-know-your-neurofilament-level/