Woot woot. Check out:
Why help theMSguide.com?
Many of you know that I started theMSguide.com as the result of a chat I had one weekend with my friend, Dr Aaron Boster. That chat lead to me taking the plunge in March 2021. Talk about not knowing what I was doing or letting myself in for…
Firstly, the channel isn’t a money-making exercise. As I don’t earn anything from YouTube it is the opposite, a personal time and money drain!
Secondly, and far more importantly, if you like the output and think it is valuable to other people with MS then I would really appreciate your help. You are helping me to run the channel and you are also helping other people with MS.
As the channel grows in popularity it is taking more and more of my time. The single best thing I can do is employ a freelance video editor to help lighten the load. Video editing is very time-consuming and it is not something I am, very good at. It is self-taught and I am sure that shows. What I am good at is interviewing people as I have a lot of contacts in the MS community around the world.
Having had MS for 29 years not and being on my 5th DMT I am struggling to keep up with the workload. I need to find an income for myself and that takes time and means it is harder still to keep up with the growing backlog of videos.
Please help here: https://www.patreon.com/theMSguide/
I am really grateful as you are helping me to help others. Thank you.
Dom
Preventing Effective Treatment Early
Preventing Effective Treatment Early
I often wonder why so many MS neurologists and their teams are so risk-averse when it comes to medicating MS hard and early. I have come to the conclusion that it is all about risk perception and the inability/unwillingness to do three things –
1: to separate out overall risk into present and future.
2: to manage what must be very difficult but necessary conversations with the patient
3: to shake the ‘doctor/nurse knows best’ mindset
My hypothesis is that there is a large element of the reluctance/inability to engage with these points is that they are related to dealing with death in care. If you’re a trauma surgeon or an oncologist, for example, you and your team will need to navigate death quite regularly, you cannot swerve involvement. But, if you’re an MS neurologist/nurse, it’s unlikely that you have to deal with reasonably regular death in care scenarios. Ergo: why would you use a drug first line that may cause death in any way shape or form? To you, the risks seem quite imbalanced. This is still a doctor/nurse centric approach because were a patient involved in the conversation, having had all the risks of MS explained to them, I think far fewer patients would opt to be so risk-averse.
Why is this important? Because in many specialities the doctor needs to make an on-the-spot decision that may pay off or may hasten death. It is a risk/reward calculation that is a serious one, but quite common. It can go either way. Sometimes it pays off and others not so much. The potential for death as a direct result of a medical intervention that they initiate is there in a way that it simply isn’t in MS neurology, and I don’t think that many MS neurologists/nurses are that comfortable stepping into that space. This hesitancy causes an internal brake, a fear: call it what you will. This scenario is all about the doctor/nurse though, not the patient.
What is about the patient is explaining risks. Not just for the now but for the duration of the disease. How many doctors/nurses can really say that they have had these tough conversations? Tough for the patient, and often scary. I daresay tough for the initiator too. How do you communicate the long-term risks? The data-driven reality is that there is an almost inevitable degree of disability that will impact the patient and all the people around them. It is made additionally difficult as the further out in time one looks the harder it is to be precise. At this stage, only broad brush data-driven remarks from datasets that are certainly not current inform this. Nonetheless, as a patient I want to know the best available evidence, I do not want reality to be varnished into something it isn’t in order to avoid the hard truths.
I know of one neurologist who tells me they make a specific point about having this hard conversation with their patients. They do it because they want the patient to understand just how screwed up they are likely to be in the future if they fail to choose an effective drug now. This is Induction therapy, the so-called flipping the pyramid approach. It is not about scaring the patient into a course of action that is unnecessarily risky nor driving them onto a high-efficacy therapy because the doctor is an ideologue. Data shows that the sooner a patient is started on a high-efficacy therapy then the better their long-term outcomes are. I can’t think of anyone who’d choose to embrace physical disability in the future if they could do something about it now.
It is the most staggeringly patronising thing a doctor/nurse can do, thinking that they know better than their patient regarding risks the patient is willing to take. The medical professionals’ job is to explain best and worst-case scenarios honestly. At the point of diagnosis, or early on in the disease, it is impossible to give a 100% reliable indication of how things will turn out (Hope for the best plan for the worst, fix the roof when the sun is shining etc). It is possible to talk about the downsides.
Whilst it is true that not everyone will have mind-numbing fatigue, need a wheelchair, catheterisation, nappies, or an anal plug because they can’t control their bowels, have issues thinking about the simplest things, have problems talking, using their hands, need countless ancillary meds for spasticity, pain, cognition, sleeping, more pain and so on. But this is the reality for many people with MS. I know several who were diagnosed when high-efficacy meds were available but were talked into ‘going gently’ because the scary unpleasant stuff was sugar-coated into the ‘things like that happen to other people’ category. Now they have many of the above issues and there is no going back.
As a doctor/nurse, just how can you be certain that your patient will avoid some or all of the above? There is no evidence that a ‘mild’ presentation now means the person is unlikely tto suffer serious effects. No way at all of telling. Everyone is operating with one eye shut. Until we have the capability to say definitively that the disease will take a particular course then it is madness to assume the best when the odds of a best-case outcome are c. 1 in 10. Who bets on odds like that? Only someone betting with someone else’s money, that’s who. A person without the disease advising someone with the disease?
I’d suggest flipping your own pyramid and asking yourself – knowing what the future of undertreated MS holds – what your own risk tolerance would be. I have a feeling you wouldn’t want to tip-toe up to your own MS and take your chances when the odds are only 10% in your favour.
Telling a patient that they have MS shouldn’t be the tough part. Helping them make the best – evidence-based – decisions now that will affect how my life goes in 10, 20, 30 years time, that is the hard bit. Perhaps it would help the doctor/nurse to imagine that they were looking after the same patient in 25 years time and having to see the effects of their approach today?
Here is an all too typical example: I know an MS patient (a fit and otherwise healthy young man) who enquired about HSCT with his MS neurologist to just have it dismissed out of hand on the grounds that it is too dangerous. The patient is a smart fellow and understands the potential risks very well. He also understands the potential payoff and considers it worth front-loading the risks for the payoff.
However, their doctor shut down the conversation then and there because the doctor felt differently.
The MS neurologist who doesn’t have MS and is not facing an uncertain future?
The MS neurologist who is not willing to allow their patient, a grown man who can choose to vote, drink, and die for his country to make an informed choice about risks now versus risks later?
That doctor is highly unlikely to be this patient’s doctor in 20 years time when their MS may have gone very badly, and is not there to see what their casual dismissal of HSCT as an option may have cost this patient. The MS neurologist was judging it all through their own lens, not that of the patient. Doctor knows best. Next patient please.
Until medical professionals see it as their duty to let the patient choose the risk they are willing to take – once fully and accurately informed – this patronisation of patients will continue. With many patients, unsure, unwilling, and unequipped to challenge, the medical professional will continue to act like a risk-averse god and choose what they think is best for their patients. That isn’t right.
Demyelination to Remyelination
Multiple Sclerosis (MS) is a demyelinating disease therefore a drug that induces remyelination ought to cure it. Pretty obvious. No?
Much in the way some people talk about HSCT (Stem Cells) as if they will fix everything with everyone I get the sense that remyelination drugs carry a similar expectation of a cure. In some cases the results may be nothing short of remarkable and in others they will be bitterly disappointing, crushing the hopes and dreams of many who have freighted remyelination with unreasonable expectations.
The reason I have been prompted to write this comes from the surprise popularity of an interview I did with Dr Will Brown from Cambridge who is part of a team researching remyelination. You can watch it here: bit.ly/Remyl-MS
I just want to inject some reality into the discussion and set expectations. The ensuing comments on the video and the threads that regularly pop up on MS Twitter got me thinking, what will remyelination actually mean for MS patients? Will it turn back the MS clock? Will I suddenly become the 53y old chap without MS that I would have been? Will I suddenly stop experiencing fatigue, coordination, eyesight issues, odd sensations and the like that are now just part of life and me?
From talking to researchers and MS specialist neurologists it sounds like a remyelinating therapy (and there will absolutely be more than one in the next 5-10 years) will have variable effects on different patients. Talking with many other patients the expectations vary from realistic to magical.
Some of the false hope is perpetuated by genuine people. After all, who doesn’t want to get better? Grasping at the press releases of small biotech companies reminds me of something my mother used to refer to it as ‘picking up fag ends’, which for those wondering are the ends of discarded cigarettes that tramps cobble together to get a tiny nicotine hit. The results are always a triumph of expectation over reality.
Rather boringly the devil is in the detail with trial results. I was reading the Atara Therapeutics press release from ECTRIMS this year and having worked in the pharmaceutical industry read it in several different ways.
Firstly, it is incredible news. Secondly, I read a hopeful and extremely carefully crafted statement that is designed to reassure current investors and attract new ones. It also wants to catch the eye of the big pharmaceutical companies as they have the infrastructure and expertise to commercialise a drug. No tiny biotech can afford huge phase 3 trials and then the lengthy and complex approvals process followed by launching and selling the drug. The aim is to be bought by a large firm for a massive amount of cash.
(It is a very expensive money-burning business to be a biotech. Spending fortunes on research funded entirely by people who hope you are right and will become stinking rich if you are. The investors are largely financial gamblers with very diverse portfolios as they know 99% of their investments will fail.)
So, I implore anyone reading these teeny tiny Phase 1&2 trial results to keep your hope and optimism but temper it with a healthy great dollop of cynicism. It simply may not work at scale, it may be deemed uneconomical and go nowhere, and and and. Drug development is a for-profit business. The drug development path is littered with promising compounds that were deemed commercially unviable and went no further.
If the stars align and everything goes perfectly then expect a further 5, more likely 10, years to pass from now (Dec 2022) before a drug is available for some lucky people. When it does it will be like the first-generation DMTs in so much as it does something but not a great deal. The first drugs on the market for remyelination will be looked at 20 years from their launch as clumsy and largely ineffective ones. That is the way.
My message is this. Be optimistic, seek solutions, and don’t expect miracles.
(Reader’s Note: I have had MS for 29y so far and would ungraciously elbow myself to the front of the queue for a remyelination drug that could turn back the MS clock.)
It Shouldn’t Be Like This (But It Is)
Go with me on this…
Someone finds a funny lump on their testicle or breast so they call the GP to book an appointment and get it checked out. Once the GP has checked it out and is suspicious, the person is catapulted onto a cancer pathway that presumes it is cancer until proven otherwise.
This happened to me recently, and in the UK this is called an ‘urgent suspected cancer referral’ and, thankfully, 90% of people do not receive a cancer diagnosis. Panic, panic, panic, and breath, no cancerous mole for me.
What about the 10% that do get a positive diagnosis of cancer? If this frightening news was treated in the way that many MS diagnoses are then the following is a rough approximation of the next steps:
Try to imagine that this newly diagnosed testicular or breast cancer patient were dispatched from clinic by the oncologist, or possibly even the oncology nursing team, with a handful of leaflets about the available drugs (some of which, if we are frank, are the modern equivalent of having surgery after a hanky with chloroform has been held to your face) and then offered an appointment in several months’ time to check how the tumour is growing and discuss options and choices.
So far, not wildly shy of the mark for many MS patients. By the way: the drugs? All of the drug options for MS sound horrendous to the uninitiated, and with no idea how to interpret the dreaded side-effects listed it is little wonder if you baulk. Grasping the leaflets about these Disease Modifying (not curing) Therapies the vast majority of patients realise that they have to learn a totally alien language at the same time as coming to terms with the diagnosis of chronic disabling disease. The faster the better. The newly diagnosed patient is on their own and with a complete freak-out diagnosis having been handed to them they do what everyone does these days and Google it despite being told to stay away from Google (for the record the most facile piece of ‘advice’ ever).
Is it lacking context? Definitely.
Are you confused? You will be.
Are you scared? Guaranteed.
Of course, that doesn’t happen with cancer (except the Google bit!). No one would dream of treating a cancer patient like this. However, that is the exact experience of far too many newly diagnosed MS patients.
Compared to the relatively well-funded oncology services in the NHS the MS service is the poor relation and when the MS patient finally gets their confirmed diagnosis of an incurable, lifelong, and progressively disabling condition there is relatively little support. The nurses are amazing but they have a ridiculous patient load.
It’s odd though. For all the patient-centricity that is talked about you still hear about the occasional diagnosis by post, the gaslighting of patients who want to get on the most efficacious therapies the soonest (a proven beyond doubt way to mitigate the long-term effects of this ghastly disease), the patients who are told to choose their own medication (you are assumed to be an expert in pharmacology, pharmacodynamics, immunology, neurodegeneration etc) and to try and get the best outcomes the MS patient is going to have to become expert in the disease and the treatments, and if they have read much they’ll know that whilst things take the time they take their brain and nervous system is deteriorating at an unknown rate. With every day that passes they are a stage nearer to a host of repeatedly proven disabilities, both physical and mental.
In case you are wondering, in the UK once cancer is confirmed there is a two-week target to start treatment. Two weeks from diagnosis. Two weeks! Not always hit I grant you but a stated ambition nonetheless.
“But (at least?) it isn’t cancer” or variations thereof are trotted out at this point as if comfort is to be taken from this spurious and slightly odd comparison. Odd, because at least many cancers are curable whilst MS remains an incurable disease. The available drugs merely – to differing degrees – modify the disease course. There is no cure. MS is progressively robbing the patient of everything they took for granted, usually when they are in the prime of life.
The sad fact is that cancer is, rightly or wrongly, strongly associated with premature death, and in our society especially, we are very scared of death. A bit like Harry Potter’s Voldemort it is customary to call it something other than what it really is. Death is powerful, frightening and to be avoided. We go so far as to publicly lionise people whom we feel have given their lives to preserve ours/others. It is called the ultimate sacrifice and valourised through the award of medals for bravery. Life is to be treasured and celebrated, the selfless giving of it for one’s fellow man doubly so.
You see, MS doesn’t kill you. You tend to die with MS and not from MS and this fact alone makes it infinitely less scary to an outsider, be that a friend or a neurologist. I can only imagine that this is the reason why MS is not taken as seriously as cancer.
Let’s return to death for a moment; the uncontested outcome, the undeniable and unavoidable endpoint for us all. I believe this is the real problem when holding the approach to MS care against that of cancer care. The focus is on the endpoint and isn’t really on the journey. MS patients are set for a long and difficult journey and yet that journey seems overlooked, devalued, unimportant when held against the fact that it is unlikely to lead to premature death. With MS the journey doesn’t seem to matter, only the denial of death.
There has been no serious systemic change in MS care, as there was with cancer treatment. Perhaps it’s time we started that conversation?
(Is the system perfect for cancer patients? Undoubtedly not. However, my point is that the professionals treating cancer or MS tend to have quite different feelings about the seriousness of the disease. This is a historical thing and the entire system surrounding the perception of the seriousness of MS is structurally flawed, or it would be taken more seriously, as a rule, not an exception.)
By: theMSguide.com with the capable help of top-notch proofreaders Rachel and Kathleen
Guest Post from New York
My friend (MSINTHEUS – on the Barts Blog) has sent me this and I agreed to publish it on theMSguide.com blog. It is an interesting take on reasons why you may not want to disclose your diagnosis. Enjoy. Any comments will be passed on as they need to remain anonymous.
Thoughts at 5 years post diagnosis
(aka what I wish I knew then, and what I want newly diagnosed people to know now. This post is an adaptation of my original post. With apologies to most readers for my unimaginative American cursing).
Introduction
When you are diagnosed with MS, you get a lot of pressure to tell people about it. That pressure does not relent. This month I have reached the five year mark since the MRI that led to a rather quick diagnosis and one thing that hasn’t changed is the unreasonable pressure to disclose to friends and family. In my case this message was continually applied by a well meaning social worker, by friends, by my doctor.
Don’t believe me? Start with the first place people will be sent to. The NMSS site for the US states: “Disclosing your MS to those closest to you — particularly those who know you well enough to know when something is wrong anyway — is the best way to rally the support you need to begin the coping process.” UK is a bit less pollyanna, stating right there on the bloody homepage: “If people know about your MS and how it affects you, they’ll be in a better place to offer support if and when you need it,” but the message is the same.
Tell people! They’re just waiting to offer support.
Not so much, people.
I am here to tell you don’t do it. Or at least think carefully before you do. It is a bell that can’t be unrung.
If you, like me, live in a real world where people do not polish turds then you might welcome a different perspective, with data backed by science. So here is a handy guide you won’t get anywhere else.
Findings
Having had significant experience with market research throughout my career, as well as interpreting and explaining medical data, I conducted a carefully set up study which comprised of one carefully chosen subject: moi. And of course even a scientific hack knows you need at least two studies to prove a thesis so I have included the experience of a friend in this analysis too with the same conclusions. The bulletproof scientific process* was as follows: I walked through every single person we had told and reviewed a few sentences on how they reacted in the moment, and over time. We then looked across these reactions and bucketed those that were similar until we found three clear themes. Therefore in this study I have come to the scientific conclusion that all people you might tell will react in one of three ways:
- The supportive, understanding person
- The weak person uncomfortable with human illness
- The toxic person who will sense weakness and take advantage
Oh, you’d like examples? I’m so glad you asked. Here are some examples of each:
Examples
Examples of reactions from supportive, understanding people
“I love you and I’m so glad you told me”.
Later asking “How are you feeling these days” and “would you like some more tequila” in the same conversation.**
Offering to accompany you to treatment, or to the doctor. Doing so for the nth time after you’ve said no each time.
Putting important things like MRIs or treatment dates on their calendars without your knowledge and magically knowing just when to reach out to see how it went.
Talking to people you know and finding out who else has this, and learning more about this weird disease that unfairly targets the super young.
Sending you random “you got this” cards, or a plant, or a “best friends” mug, or a “fuck you, ms” shirt for no reason at all
Without any fanfare, using the Facebook fundraiser to raise money for MS research when it’s your birthday
Randomly sending you articles of new science that may help. (Note I said science peeps – not yoga poses or kombucha recipes).
Not treating you like a delicate flower, and still coming to you with their own problems – or concert tickets, because we all have our shit, and we all need a safe space to forget it for a bit.
And if you really want to know who your friends are wait until MS is in the news, like when the Regeneron covid antibodies were approved in the US for prophylactic use on high risk individuals, or when a celeb is diagnosed. The people that text you that article asking “can you get this”? The people that learn about celeb diagnoses, and immediately start following them for you on Instagram trying to get a connection? THOSE are your people, peeps.
Examples of weak people who are uncomfortable with human illness
These people are actually very easy to spot in hindsight, unfortunately they’re usually people you thought would fall into bucket one, and then they disappoint you with their cowardice and inability to help due to their own personal discomfort. The closer they are to you, the more it will hurt.
Abandonment from a family such as a parent or inlaw who falls into this category is particularly insidious and painful, which is why I strongly recommend waiting to disclose if that kind of reaction will do more harm than you can handle at the time. Remember, stress makes MS worse so if telling someone will worsen your health then definitely don’t do it!
These people are very easy to identify in hindsight. Common reactions include:
Saying all the right things on the phone, then never speaking to you again.
Suddenly stopping inviting you to things
Avoiding you
No more texts, or calls, or emails – about anything
Ghosting you
Sensing a theme, peeps? We did too.
Examples:
I had a friend who I had a lot of fun with and thought was close to who I told. She was nice and talked to me and would check in on how I was feeling, but she stopped inviting me out to things. I lost a big social outlet, at a time when I desperately needed some fun.
I reluctantly told some in laws, after years of telling no one on that side of the family, because their resentment at my perceived excessive Covid precautions made it necessary and I did not want them to take my refusal to get together personally. After hearing the news on the phone and asking some questions, the phone call was cut off due to my brains’s failure to properly estimate my phone’s sad battery capacity. I kept my promise to follow up as soon as charged but that call was met with a text saying they were at lunch and would call me another time. Which of course never came. It was radio silence from that point on. No “I can’t believe you’ve been going through this and we didn’t know, how can we help?” No, “I’m so sorry this happened to you, thank you for telling us.” I was even ignored at in-person events from then on, they even snuck into Manhattan without telling me and made plans to see my husband behind my back! While I know it’s not personal, that doesn’t stop me from feeling deep pain and hurt. It’s hard not to take something like that personally. I very much wish I had never said anything.
So, if you – like me- think you will not enjoy the cold shoulder, or being treated like a leper, by someone who is supposed to be your family or your friend, you might want to hold off on the disclosure. MS is stressful enough without other people hurting you and causing you stress and grief because of their own unprocessed discomfort with illness.
Examples of reactions from toxic people who will sense weakness and take advantage
Some of these have happened to us, and some of them outside the “study”. But these are all real examples, and they do happen. These people exist, and they actively and intentionally will do things to your detriment. Examples:
An employer may cite “performance reasons” for an eventual termination (this has happened to people, be VERY careful before disclosing to an employer or a friend who is also a coworker. The misinformed make damaging assumptions)
A landlord suddenly raises your rent when you cite diagnosis and being in the hospital as the reason for the ONE TIME in years that you were late (this happened to a friend). Sometimes you just have to be smart and aware. Your weakness is someone else’s opportunity.
A spouse may realize you may be dependent on them one day and may use that knowledge to become abusive, cheat, steal, generally mistreat you in other ways they would not have tried had you not been weak, or all of the above. Sad, but it happens.
A parent disinherits you, stops speaking to you, or acts in other ways that actively cause you harm. This happened to both myself and someone I know. All the books say your parents want to help, especially when you are still relatively young, but none of the “helpful resources” out there that I have seen even remotely acknowledge that not everyone comes from perfect families and toxic narcissists can be found amongst parents, too. In my case the disinheritance and immediate communication cutoff was promoted by a request for a small loan I foolishly made, then the actions were rationalized by made up fabrications of things I had never and would never do. Yes, people! If you have MS you officially have the most expensive disease in the world. According to most research 70% of people are no longer employed after ten years. Yes, a diagnosis is shocking and life changing and you may need some help with unplanned hospital bills or time forced off work. But how dare you ask your parents for any financial support! I mean, seriously, how selfish can you be?
A note on children
Everyone says “tell your kids right away!” As with all parenting advice, this is right for some kids, and not for others.
MS may be a life changing crap diagnosis but it doesn’t have a magic wand that magically takes away your instincts as a parent. Keep being a parent. That means doing what you think is best for YOUR child. Think you want to tell them? Great! There are TONS of resources to help you with that. Read them, decide for yourself if they make sense. Use them, or don’t.
Don’t want to tell them? You know your kid best! In both myself and my friends’ cases we were under great pressure to tell our children. We had young, anxious kids, who craved and needed normalcy. People didn’t understand. “They should know”, said “experts”. In both our cases we held firm, and parented as we always had. In both our cases we were met with great shame and pressure to make a different decision.
When each of us finally told our children, they were old enough to handle the news. We also both realized there is a lot less anxiety that comes with “I have this and I’ve taken this medicine for three years, and so you can see that I’m ok, right”? vs “I just learned I have this and they’re advising I take this medicine and we’ll hope it works”. The latter would have been way too scary for my child. Telling her when she knew everything would be okay took the fear out of the information because I waited until the unknown and unpredictable was known and predictable. Turns out, predictably in their parents is a very reassuring thing to kids. Who knew! I stuck to my guns, but it would have been much nicer if I didn’t have so much damn pressure and even in some cases shame from people for not handling things the way they thought I should.
Conclusion
In conclusion, before you disclose, THINK. Think about why you are telling that person? What do you hope to gain? What of the three buckets will they fall into? Everyone assumes everyone falls into the first bucket, and for many people most do.
But we’d be doing people a huge disservice if we did not acknowledge that this isn’t true for everyone, for some people reality does not reflect this and that is why you have me, to tell you the unfiltered truth. Really think about who this person is, and how they might react. Will you gain more than you may lose? Are you ok if they end up falling into a different bucket than you had hoped? Are they in a position to cause you real harm if they fell into the last bucket?
Please seek out advice, as needed. But take all advice with a grain of salt. The reality is that no one likes to talk about this unpleasant stuff. And MS has a tendency to bring out the unpleasant in people.
So if you remember only one thing, remember this: NO ONE GETS TO TELL YOU HOW TO “DO” MS.
However you decide to handle it, that is the right way to proceed.
SCIENTIFIC FOOTNOTES
*Because I believe in writing responsibly, I feel compelled to say out loud this is sarcasm, for those of you daft enough to have not yet figured that out. Despite the obvious (please let it be obvious) use of hyperbole for a little fun the conclusions, however, are real, as unscientific as they may be.
**We may have been dealt a shit hand but FFS we’re not dead, people.
Roadtrip!
Or, as I soon realised, it is all about having a purpose in life.
My good mate from University has a monumentally flaky girlfriend and they had planned this weekend as a lovely 3 days of walking in the most beautiful of places, the Lake District. For his birthday next Monday. And she bailed last night. Cue a phone call to Dom: can I go walking in the Lakes for several days with nearly all expenses paid, leave Sunday morning? Hell to the yes I can.
But it’s not really all about helping out a mate. It is the planning a road trip at the last moment element which is also fun for me, and very purposeful. Knocking out a few Wainwrights and Scafell Pike (pictured above) in mid-November is not without a host of weather-related hazards. I mean, who wants to suffer the indignity of being helicoptered off or having a Mountain Rescue team have to locate me because I have been an absolute cretin? This means I get to get the right OS map sheets, assemble my winter hillwalking kit, get the appropriately sized rucksack from my embarrassingly large one for every occasion collection, reproof my waterproofs, apply yet another coating of Leder-Gris to my trusty Altbergs, do an inventory of my gear, and bake two loaves of bread because we are self-catering in a camping pod in Borrowdale. Oh, I also need to check and adjust the tyre pressures in my car for the 6h drive and add my mate to my insurance. And get him a birthday card for next Monday because it wouldn’t be very sporting to wake up on Monday and forget the poor sods birthday?
I have had to cancel an interview on Saturday, will have to make a short video for theMSguide.com explaining that normal service (a Friday release of something good is what I promised; like voluntarily putting a gun to my own head but if I don’t have pressure/expectations/purpose then I am a lazy bugger) will be interrupted.
MS wise this is a ‘good thing’ because I have a firmly held belief that ensuring I have a purpose is critical to staying well. The fact that much of my purpose is focused on physical activity is a happy accident for my MS. There have been a few times in my life when I have allowed myself to drift and that way lies dragons. Dragons of inactivity, listlessness and mental anguish. Seriously, it is very bad for ones mental health to lack purpose. You can rapidly go to some very dark places where it can get very Hotel California very fast. And if that last remark puzzles you then imagine me sighing deeply, remarking about the youth of today etc and then reminding you of the immortal line, “Welcome to the Hotel California…where you can check out but you can never leave”.
I usually loathe stories with a moral but I will temporarily overlook that for a moment because the moral of this post is that if you don’t want to slide all too easily into a spiral of inactivity and mental health issues then it is critical that you have a purpose in your life. And in case you were hoping that someone or something is going to come along and give you that purpose then you are deluding yourself. Purpose comes from within and you need to construct it from what is there. In my case, today, it is helping out a chum and going walking in an amazing location.
Here endeth the sermon, I shall dismount from my soapbox and bid you adieu. I’m off to the Lakes and there is a lot to do before I leave.
Disclosure
Disclosure seems to be the theme of many MS strands at the moment, so I thought I’d add my two-penn’orth. My only advantage is greater hindsight as I was diagnosed with MS 28y ago. More than half my life has been lived with the diagnosis and it is fair to say that it has influenced every single aspect of my life. Recently, I started to reflect on what that has meant.
Some insights are very gratifying and others are very hard to even think about. MS has alternately made me a much better person and, at times, quite the arsehole. I want to blame the bad times on the MS but I think it was in me and, at best, I can only involve MS in my rotten deeds and not blame it all on it.
However, there are things I am extremely proud of that offset the episodes which make me cringe and I take comfort in the knowledge that there are far more of the former than the latter. I’m 52 now, so a fair amount of time has passed and it turns out that the cliche is true. Time is a great healer.
What I am really saying to you is that it takes time to come to terms with your MS. I wouldn’t say I welcome it into my life but I am comfortable with its presence. The issue with disclosure, especially when it is all new to you, is that you need to jump ahead a bit so that you can ensure it is not frightening to others.
While you remain afraid of your own MS – and it makes perfect sense to be frightened of it; like skydiving is naturally concerning the first time – you’ll find it extremely hard not to communicate that fear to other people. Whether they be someone you fancy going out with or working for it will be the same, your fear leaks out. We’ve all seen it in others or experienced it ourselves. You can’t help but betray your anxiety. I am still petrified of bloody wasps (what IS their point?) and swat and wave at them. I then get some smart alec saying, ‘They can sense your fear’. This may be true, but I’m petrified of the damn things and it is a very rational fear in my mind.
So MS and disclosure? What useful addition to the discussion can I make? It is blunt so brace yourself. You need to get a hold of your MS and how it sits with you. Until you can stop being afraid of your MS it is very difficult to avoid communicating that concern to others. Whomever they may be.
I resolved from Week Two to just plough ahead with life as I always have. If something has scared me (apart from wasps) I have confronted it head-on. Skydiving, big drops when skiing, hard climbs on the bicycle, scary climbing moves, dealing with aggressive idiots etc. the more you do this, like anything, the easier it becomes. In this case, it is managing your own fears.
So I urge you: get therapy of some kind. See a professional, chat it over with your best friend, join a group (shift.ms or esupporthealth.com), go bungee jumping, come out using a video on LinkedIn (As my mate did recently. Six mo. after her diagnosis she owned it so no one else could put their spin on her story) but confront it, accept it and cure your fear of it because ‘it’ ain’t going anywhere.
EDIT:
I’d like to thank my friend Kay for reminding me of something obvious I missed. Both she and I took it upon ourselves to give truth to another cliche: knowledge is power. We both got head down into researching and understanding MS from a patient perspective. This had led me to starting theMSguide.com in March of this year and more patient ambassador type roles. That is the really unexpectedly good and fulfilling thing from ths bloody disease. The idea that I can use my experiences to help others is very gratifying.
( this piece also appears on the Barts blog here: https://multiple-sclerosis-research.org/2021/10/disclosure/ )
Patient Involvement, Or Not?
Where is the patient involvement in designing the DMT guidelines for Multiple Sclerosis?
According to the NHS: ‘People and communities are important to us because they help us improve all aspects of health care, including patient safety, patient experience and health outcomes – giving people the power to live healthier lives.’
The NHS England algorithm for using DMT’s says: ‘The purpose of this algorithm is to provide a framework to aid decision-making for multiple sclerosis (MS) specialists and patients, to help reduce excessive variation in practice, and ensure safe and effective prescribing. It is understood that there may be situations where there is no single ‘right’ or ‘wrong’ therapeutic approach, and different experts may reasonably hold different views. ‘
Despite these unequivocal statements regarding ‘the patient’, Multiple Sclerosis patients have no input whatsoever into the decision making process about what drugs are used in MS and when. It is as if the treatment of multiple sclerosis is so complicated, the syntax so specialised, that unless one is a specialised neurologist or similar then comprehension is simply beyond them.
Keeping the patient voice out of one of the single most important areas of our treatment speaks to the very old fashioned patrician ‘Doctor knows best’ attitude. This gives the rhetoric around patient involvement a very hollow sound. Before the reply is made about MS Charity consultation reflecting the patient let’s put this to bed too. There are so very few patients with Multiple Sclerosis employed by these charities that when they claim to speak about the patient experience, that also rings hollow. Sure, you can ask them for input, to reflect patient attitudes etc but the replies you will get are mediated by people who do not have MS and, try as they might, can’t accurately reflect the patient experience.
If genuine patient involvement in MS care is to be more than just a phrase uttered by policymakers, to salve their own ears, by hearing themselves say it out loud at every available opportunity, then MS patients need to be directly involved in designing the NHS DMT prescribing algorithm. Repeated second-hand ad-hoc personal experiences or the representations made by well-meaning intermediaries are not a reliable or genuine substitute for including patients. Patient with lived experience of MS must be at the table and involved in both the discussion and the output.
Until there is unmediated patient involvement in the construction of the prescribing algorithm, it is difficult to understand how the experts in MS patient care can do this while knowing full-well of the failure to involve the very patients who will take these treatments in the decision-making process. We, patients, are a very strange and diverse bunch when compared to the comparative uniformity of highly educated and very scientifically/technically/financially learned people who decide about drugs for our use created. The issues caused by allowing patients into the hallowed backrooms of clinical decision making are many and varied. Heck, I imagine disabled persons access/accommodation would rocket near the top of the agenda! These are not insurmountable hurdles, just different challenges.
Putting the patient’s names on the guidelines, having actual patient input into them is the very least we ought to expect, not the most we can hope for.
Dear NHS, we want to be involved in the way that you say we should.
You talk the talk, but will you walk the walk?
Visualising the future of a patient’s MS is getting easier by the day
The concept of ‘was that my last good day’ is a permanent spectre in my life. I no longer get as rattled by the unpredictability in quite the way that I used to, but it never really goes away. For example: I had an amazing weekend just gone. I Walked 29km over two days, went to a pub for the first time since lockdown, baked some fresh bread, saw friends etc. And now, Monday morning, I wake feeling a bit weird and a bit off. Hard to explain but my mood is one of inexplicable hopelessness, I feel shattered already and am generally quite sub-par. Go figure.
One of the stranger things about having MS is that you just have to accept is the complete unpredictability of it all. Hot/cold, happy/sad, pain/no pain. see/double vision, you get the idea. If you don’t I reckon you’ll go stark staring mad in a matter of months. But back to the present wobble…
All of a sudden, across my mind, flits the well worn thought of, ‘was that it’. Rational Me knows that this is ridiculous. Still, rationality takes a back seat and Irrational Me triumphs. I know this is a bad and dark hole to allow myself to be dragged into and it is a Herculean effort to force Rational Me back and send it on the daily task of kicking all the silly Irrational Me thoughts and fears back into the dark recess where I think they ought to stay.
Talking of dark holes, these are the parts of the mind that don’t show up on my MRI and are not easily quantifiable to my neurologist. They are impossibly hard to describe and when I get to my once annual review they seem like an odd abstract thought that, in trying vainly to describe, will take away from that valued visit for the ‘serious stuff’, making me loath to spend those precious minutes trying to explain the inexplicable.
There are so many things to measure with MS, and the neurologists want to hear about them because that is an efficient clinic visit. Recording the measurables. How well you walk, pee, see, swallow, and so on. They like those sort of metrics as they can place you somewhere, measure stability or decline and tell you where you are in the journey of decline. The anxiety stuff? The demons, the black feelings and so on? Most prefer to leave that to the staff of P-Wing because there is no EDSS equivalent that can describe the daily rollercoaster of emotions, that’s life. I always leave feeling as if everything that has been said is caveated with the equivalent of a warning on an investment product about the past performance being no guarantee of the future.
Annoying as that is to both parties, in Multiple Sclerosis there has never really been a way to look into the future and reliably predict either the potential onset, extent, and/or severity of the illness in general or the relapses that characterise the earlier stages of the disease. So when they say that it is impossible to tell, they aren’t joking. Watch and wait is their motto. Hope and pray is mine. Either way, both are as uncertain as the other. They can measure what has happened or, at best, what is happening, and in fairness, who likes dealing in the what-ifs and the maybes? I imagine that every neurologist that has ever had to deliver a diagnosis of MS to some poor soul has been met with a version of, “what is going to happen to me?” and it is a very difficult question to answer. The ability to quantify anything with regards to that question is v tricky, and, in general, by the time a doctor has made it to the heady heights of Consultant they are well-versed in the delivery of difficult messages such as, hmmm, not sure really, we’ll have to wait and see. No looking into the future here. Move along.
But there are some glimmers of hope! Whilst there isn’t the precision that I or my neurologist may want, these days there are tools that offer the opportunity to go beyond an educated guess.
I can think of three emerging tools that give real hope for taking a forward view. Neurofilament Lightchains (NfL’s), Optical Coherence Tomography (OCT), and Artificial Intelligence (AI) analysis of MRI.
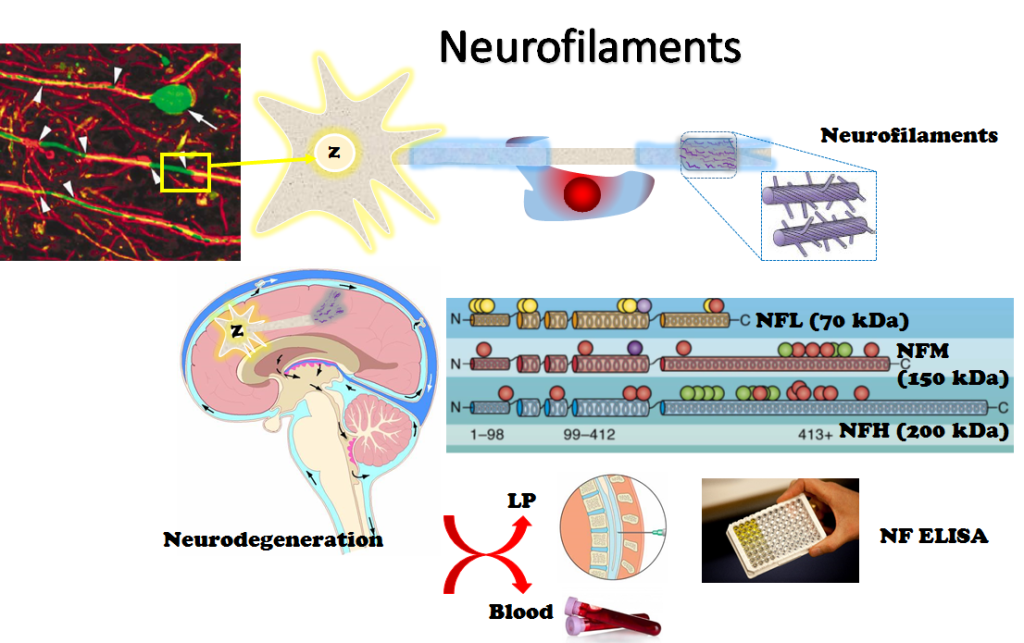
1 – Starting with NfL’s, these are things that can be taken from the fluid that is drained during a lumbar puncture. They serve as biomarkers, a fancy way of saying signposts from our body, regarding three main things:
- Risk of progression. E.g.: The how bad is this going to be doc, question?
- Clinical disease activity. Not what you can or can’t see/elicit from patient recollection of symptoms or tests done to determine the level of effect at the time but what is actually going on in my noggin.
- Treatment response. Have you ever wondered if the DMT you are on is doing anything? I have a standard reply to people when they ask about DMTs for MS. I explain that unlike a paracetamol that does or doesn’t fix a pain, the DMT is taken with a belief in science and large scale clinical trials. They say it works and I have to believe that.The neurologists are in the same boat. We all have to believe in science that a good DMT increases the time between relapses and reduces the effects of a relapse when we do have them. We will, it is a progressive illness. A very rare few may experience no measurable progression in life. They are the exception that proves the rule.
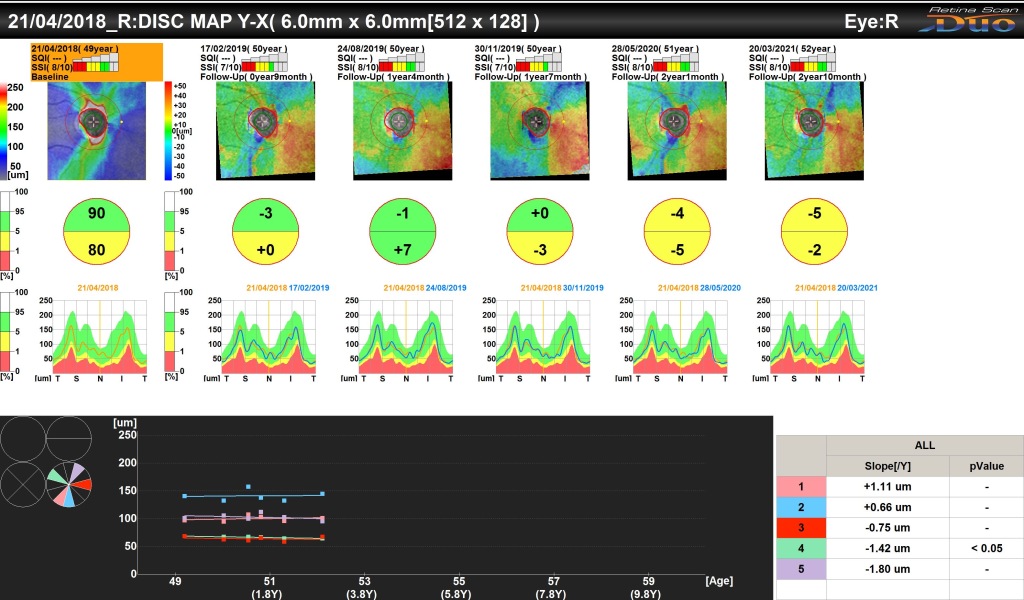
2 – OCT scans are a bit like looking into a supermarket barcode scanner when you have one. It feels like little bars of red light flitting around trying to determine the price of your eyes! What comes out though is amazing. They map the retina thickness and condition and compiled over time they allow an expert to see into the brain through the eyes. The presence or loss of ganglion cells (I am emphatically not an expert) also serve to let the doctor know what is happening in the brains of the patient. When they are done as a matter of course (not right now) they’ll also need someone to understand and interpret them, or they are pointless – this probably isn’t going to be your neurologist.
Presently, it still does not make a difference for the clinical management. But it’s very promising and much more convenient than brain volume measurements on MRI, and is probably going become very important in the future.
This is a very promising biomarker as it is easily accessible and reflects brain damage and will allow the neurologist to quantify how neuroprotective a treatment is.

3 – Finally, AI examination of MRI scans is allowing doctors to identify different manifestations of MS. By seeing these they can better understand what is more likely to happen. An added bonus is that once a computer is sufficiently well trained and is running the right software it can be relentless. Humans get tired, need coffee, are distracted, miss things, misinterpret things, however diligent we are. People try their best but it is a boring and repetitive task gazing at slice after slice after slice of an MRI. To have a computer do that heavy lifting is infinitely preferable. This means that the human expert neuroradiologists get notified of the results and can verify and check the anomalies a computer picks-up that may go unnoticed to a human being, however good they are.

If you aren’t a little in awe by now then you need to get checked. This is amazing. For the very first time, there are tools and technologies that will allow our doctors to treat us for what they know is going to happen and not what they think might happen. It is the moving to precision treatment and not hitting everything with the biggest hammer they can lay their hands on. It is allowing patients to understand why their neurologists offer the choices they do and say some of the things they do. These days, only the most backward neurologists think MS is an on/off sort of disease. To say you aren’t progressing is inaccurate. A better phrase is, ‘with the tech we have available we can’t see anything at the moment.’
These tools are years away, not decades. The next time I see my neurologist I’ll be asking them how they think they’ll be deploying these technologies to treat me better? As for the mental strains, I still don’t know where to begin with these. I have found that it is likely to remain my job for a long time to come. But things do get a little easier when we know a bit more about what is around the corner. Go science!
With thanks to Dr Sharmilee Gnanapavan (@neurognanapavan) and Dr Ide Smets (@SmetsIde) for ensuring I wasn’t talking total rubbish.
For some more in-depth reading there are links to some of the most recent work:
NfL’s – https://multiple-sclerosis-research.org/2021/04/do-you-know-your-neurofilament-level/